Introduction
In today’s hyperconnected world, medical information is abundant but not always accurate. Social media, messaging apps, and content platforms have transformed how people access health information. Unfortunately, these channels also enable the rapid spread of misleading or false cancer-related content. For oncology patients, this can create confusion, fear, and in some cases, dangerous delays in care.
As cancer diagnoses trigger urgent decision-making, the search for answers often leads patients to unverified online sources. From viral claims about miracle foods to fear-inducing videos discouraging chemotherapy, digital misinformation can interfere with timely, evidence-based care. For oncologists, the challenge is no longer limited to clinical care, it now includes a digital front where truth must be defended.
“Every time a patient chooses misinformation over medical advice, we lose more than time—we risk outcomes.”
– Dr. Ashok Rao, Surgical Oncologist
How Misinformation Impacts Cancer Patients
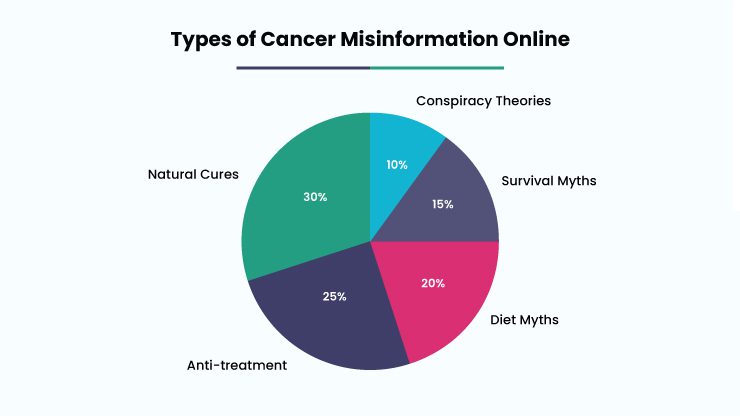
The emotional weight of a cancer diagnosis makes patients particularly vulnerable to misinformation. According to a JAMA Oncology study, nearly one-third of high-traffic cancer articles shared on social platforms include inaccurate claims. Some common examples include:
- Promoting turmeric or alkaline diets as cancer cures
- Urging patients to stop chemotherapy or radiation
- Suggesting doctors are hiding “natural” remedies
- Framing emotional trauma as the root cause of cancer
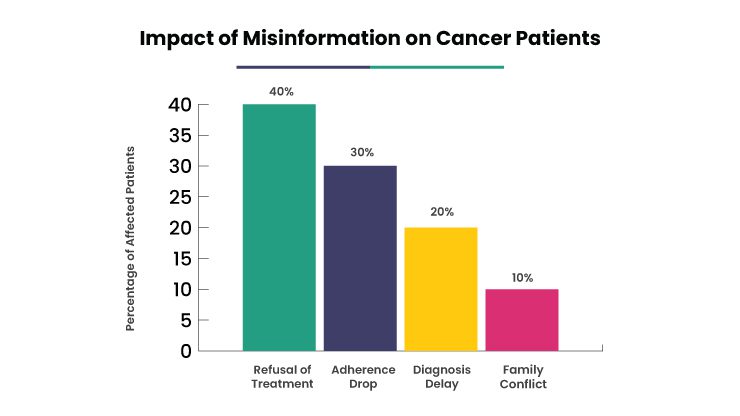
Such misinformation can have significant consequences:
- Delays in treatment as patients pursue unproven methods
- Non-adherence to prescribed therapies
- Increased psychological stress from conflicting advice
- Family disputes over treatment decisions
In many cases, this content is crafted not out of ignorance, but for profit, capitalizing on the fears of patients in search of hope.
Recognizing Common Cancer Myths
Understanding which myths are circulating allows healthcare professionals to address them directly. Examples include:
- “Chemotherapy does more harm than good.”
- “Cancer feeds on sugar- eliminate all carbs.”
- “A positive attitude can cure cancer.”
- “Cancer is always caused by unresolved emotions.”
- “Natural remedies can replace clinical treatments.”
These beliefs often gain traction because they sound simple or comforting especially compared to the complexity of medical treatments. Cultural influences, traumatic medical experiences, and misinformation from trusted community voices can reinforce them further.
Digital Strategies to Combat Misinformation
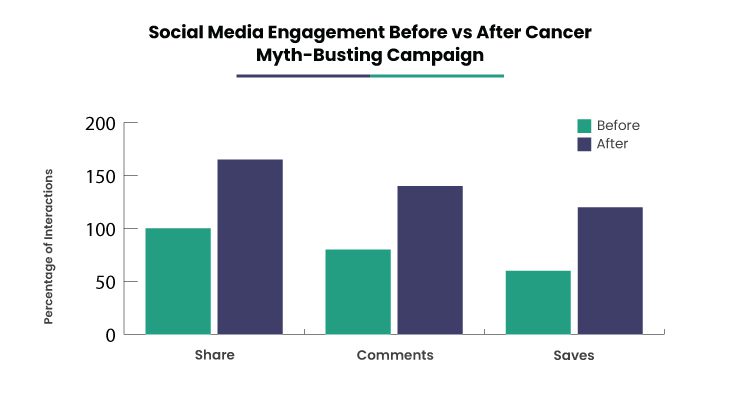
1. Social Media Campaigns: Bite-Sized Education
Platforms like Instagram and Facebook are ideal for quick myth-busting content. Oncologists or clinics can run regular series such as:
- “Myth vs Fact” carousels
- Short explainer videos or reels
- Weekly themes like #MythMonday or #FactFriday
A Mumbai cancer center’s bilingual myth-busting reels saw a 70% rise in engagement over six months.
2. YouTube: In-Depth Clarifications
YouTube allows for longer, more nuanced explanations of cancer topics. Formats that work well include:
- “Ask the Oncologist” Q&A videos
- Animated whiteboard sessions explaining complex concepts
- Interviews with survivors who share their experiences with misinformation
Tips: Keep videos under 10 minutes, include local-language subtitles, and use empathetic language.
3. Partnering with Survivors and Influencers
Collaborating with cancer survivors who have a social media presence helps spread accurate information with a personal touch. Formats include:
- Joint Instagram Live sessions
- Co-authored blog posts
- Video testimonials about choosing evidence-based treatment
Always maintain ethical clarity and disclose that content is not a substitute for medical consultation.
4. Live Q&A and Webinars
Interactive formats like webinars or livestreams allow real-time myth-busting while building rapport with the audience. Examples:
- “Ask Me Anything” monthly sessions
- Focused myth-busting by cancer type (e.g., breast cancer)
- Multidisciplinary panels including oncologists, psychologists, and dietitians
Patient questions often reveal trending myths and help inform future content.
5. Expanding to Emerging Digital Channels
Misinformation thrives not only on mainstream platforms but also in:
- Telegram groups
- Reddit communities (like r/cancer)
- Quora discussions
- TikTok videos
Young, digitally savvy oncologists can play a vital role by providing clear, compassionate responses in these forums especially in local languages.
6. Educational Newsletters and Digital Guides
Newsletters offer a private, focused way to share accurate information:
- “Myth of the Month” features
- Easy-to-read research summaries
- Patient stories dealing with misinformation
Downloadable guides like “10 Cancer Myths Debunked by Doctors” can be shared across age groups, including elders who may not use social media.
Debunk with Empathy, Not Aggression
Ethical communication is essential. Oncologists should aim to:
- Address the myth, not attack the believer
- Avoid naming individuals spreading misinformation
- Use references from WHO, NCI, or peer-reviewed sources
- Encourage patients to ask questions during appointments
“Clarity, not confrontation, is what changes minds.”
– Dr. Namrata Pillai, Medical Ethicist
Case Study: A Local Campaign with Big Impact
In 2023, a district hospital in Odisha faced a surge in chemotherapy refusals due to a viral WhatsApp message. In response, the hospital launched a local digital awareness campaign using:
- Facebook posts in Odia
- Local radio broadcasts
- Staff training to address myths
Results:
- 30% increase in chemotherapy uptake
- Helpline traffic doubled
- Patient trust and satisfaction improved
Even small, localized campaigns can yield substantial improvements when rooted in community needs.
The Institutional Role in Myth-Busting
Beyond individual clinicians, hospitals and medical associations must lead the fight against misinformation by:
- Hosting multilingual online myth-busting resources
- Collaborating on government-led digital literacy campaigns
- Training staff to gently counter misinformation
- Issuing monthly myth trend reports
Professional associations should also support digital outreach through clear ethical guidelines and digital engagement training.
Empowering Oncologists as Digital Educators
Barriers such as limited time, tech skills, or fear of online backlash can discourage oncologists from digital outreach. But institutional support can change that:
- Provide short digital communication training
- Offer pre-designed myth-busting templates
- Assign communication officers to assist clinicians
- Create cross-disciplinary support teams
When provided mentorship and tools, even the most tech-averse doctors can find their digital voice.
Future Forward: Using AI to Track and Counter Misinformation
Artificial intelligence offers exciting tools for health communication:
- Social listening tools to detect viral myths early
- Language-specific chatbots answering common questions
- Browser extensions or filters that flag false claims
- Myth-correcting pop-ups on WhatsApp or community forums (in development)
If used ethically and transparently, AI can be a powerful ally in public health education.
Conclusion: Restoring Trust, One Truth at a Time
In oncology, information is not just a support tool, it can be lifesaving. As misinformation grows, so does the responsibility of oncologists to step into the digital space as educators and advocates.
Through empathy-driven outreach and strategic use of digital tools, oncologists can help patients make informed, confident decisions guided by facts, not fear.
In the digital age, accurate medical knowledge is a form of care. And every myth we dispel brings patients one step closer to healing.